
Digital transformation and the productivity and efficiency challenge
Barriers to productivity gains
Despite the promise of new technologies, it is essential that trust leaders (digital or otherwise) are not naïve to the challenge of deriving benefits from them. Ultimately, the tech alone will not come to the rescue of sliding NHS productivity. And in fact in some cases, when done badly, can make things worse.
Health Foundation technology impact study
In 2024, the Health Foundation commissioned a rapid review of the impact of technology on staff time in health care, sampling 467 studies from between 2010 and 2023 that looked at whether a particular technology saved staff time (Shemesh et al, 2025). The data is striking.
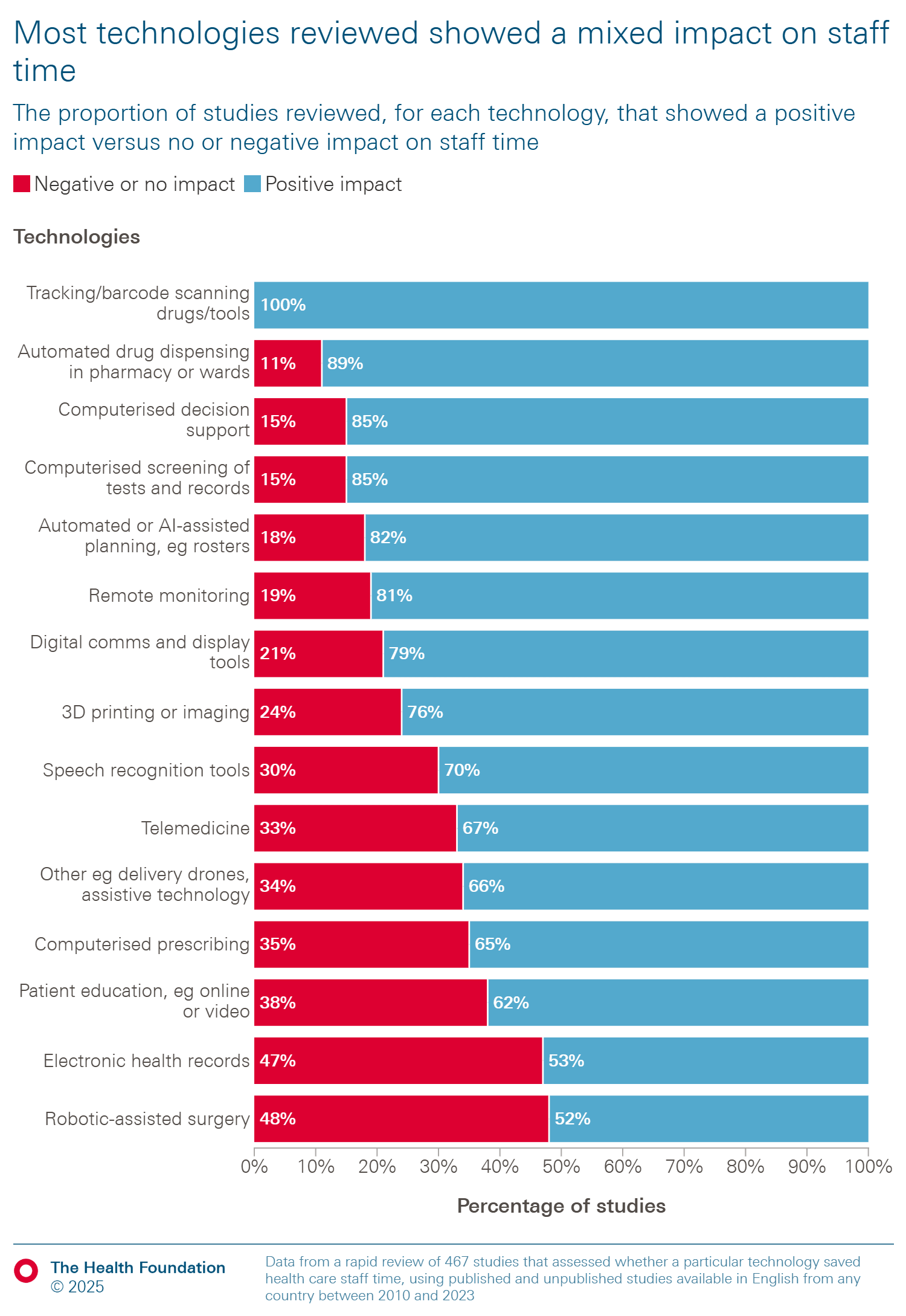
As the graphic illustrates, the impact of each of the listed technologies on staff time is generally mixed. Every technology, except for tracking/barcode scanning for drugs/tools, has some instances where it has saved staff time and others where it has failed to do so.
It’s perhaps no surprise that Electronic Patient Records (EPRs) are 50/50. As we’ve written before, there is a strong dependency on the way that EPRs are implemented. Research by NHS England and KLAS has shown that usability varies wildly even among trusts using the same system. This is because as well as the quality of individual products, there is also a dependency on how well any software is implemented. Work by the Royal College of Physicians has shown how different the experience can be across different settings (Kinderlerer, 2024).
EPRs can save staff time by centralising clinical information. However, in practice, in many ‘best of breed’ type implementations records are often fragmented across services, wards and platforms and require multiple logins for access, which can negatively impact staff time. You can read our previous leadership guide with analysis on the EPR challenge (NHS Providers, 2023).
As the Health Foundation highlights, "just because a technology had a negative impact or no impact on staff time does not imply it was unsuccessful overall. Technology might have a negative impact on one aspect of a journey but still, for example, improve clinical outcomes, promote patient safety or enhance patient and/or staff experience". So when assessing the benefits of a particular intervention it’s important to look at that in the round to see overall impact on productivity.
Environment factors leaders should consider
The challenges of driving productivity benefits from technology have attracted attention for some time. The NASSS framework was developed in 2017 by Professor Trish Greenhalgh (et al) (Greenhalgh et al 2017) and offers a structured way to consider the success factors for technology in health and social care settings. NASSS stands for Non-adoption, Abandonment, and challenges to the Scale-up, Spread, and Sustainability of health and care technologies. This work again recognises that technological success is about how well it fits within complex, real-world systems. It highlights multiple interacting domains that influence whether a digital health intervention will be adopted and sustained.
The factors and their domains include:
The condition
How complex is the condition (e.g. based on comorbidities etc)? The more complex the condition the more difficult it is to implement digital tools, as they are often point solutions or single condition based.
The technology
How is the approach to product design and quality impacting usability? How is the technical approach (e.g. to information security, or uptime) impacting reliability?
The value proposition (to patients, staff, and funders)
Is the technology solving a known and evidenced problem, or merely the latest intervention rolling off the hype cycle?
The adopter system (the users and their readiness)
What skills or abilities are expected of the patient or caregiver in terms of the use of a new technology? What attitudes might patients or staff have to the technology in question? In the latter case, will it threaten their jobs?
The organisation (culture, capacity, workflows)
What is the organisation’s capacity and readiness to embrace new technologies? What changes to established workflows are required? Organisations with a supportive culture, strong leadership and adequate resources will have greater readiness to implement digital tools, and face less challenges when doing so.
The wider context (regulation, policy, infrastructure)
Are there clear regulations and interoperability standards already in place? Public and professional attitudes towards the technology is also a key consideration influencing the adoption and sustained use of the technology.
Embedding and adapting over time
How much scope is there for iterating and learning as the technology, context and user needs evolve over time? Is continuous learning and adaptation encouraged and prioritised?
This framework can be a useful tool in assessing the difficulty of implementing a particular piece of technology. By systematically considering the environmental factors that may make things easier or more difficult for digital change, trust leaders can have a structured conversation around this to ensure that they are fully accounting for some of the barriers that tend to arise. This will help them plan properly for what’s ahead.